Have any questions?
- ServiceNow
Ready to Transform Your Business — Risk-Free?
Start with a 30-day trial and experience the value before you pay.
- DevOpsCloud Implementation Services
At LiimraSoft, we bring years of deep, hands-on expertise in cloud computing—across AWS, Microsoft Azure, and Google Cloud—to help organizations unlock the full potential of high-performance cloud environments. Whether you're building in the public, private, or hybrid cloud, we design and implement solutions that are secure, scalable, and aligned with your business goals.
AssessOperateOptimizeScale / EvolveReady to Transform Your Business — Risk-Free?
Start with a 30-day trial and experience the value before you pay.
- Automotive
- Digital Marketing
The Leading Platform for Growing Practices
See How LiimraSoft Can Grow Your Practice
Ready to attract more patients, improve your online presence, and scale your clinic with confidence? In just 20 minutes, we’ll walk you through how our healthcare marketing platform helps medical and dental practices thrive.
- IT Consulting
Information Security
IT security refers to the protection of digital information from unauthorized access, theft, damage, or any other malicious activity.
Cyber Security Service
Cybersecurity refers to the practice of protecting computers, servers, mobile devices, electronic systems, networks, and data from digital attacks, theft, damage, or any other malicious activity.
Data Center
we provide a range of data center services to help businesses manage their IT infrastructure.
Networking & Connectivity
We specialize in creating custom technology solutions by combining hardware, software, and services from multiple vendors into a cohesive and functional system
Cloud Security
Regardless if you already have a well-established cloud security program or are starting your cloud migration for the first time, we can help you enhance your security strategy.
Help & Support
We are passionate about your business, we make sure your issues are resolved in timely manner and your services are available and running error free.Ready to Transform Your Business — Risk-Free?
Start with a 30-day trial and experience the value before you pay.
Dental Insurance Eligibility Verification
Accurate. Efficient. Patient-Focused.
Verifying dental insurance eligibility is a critical first step in the revenue cycle—and one of the most common sources of billing errors and claim denials.
What Is Dental Insurance Eligibility Verification?
Dental insurance eligibility verification is the process of checking a patient’s insurance coverage before their dental appointment.
It ensures that their insurance plan is active and confirms what treatments are covered, how much is paid by insurance, and what the patient may owe.
- Confirms the patient’s insurance is active
- Identifies covered procedures and limitations
- Helps provide accurate cost estimates
- Prevents claim denials and delays
- Improves patient satisfaction and office efficiency

Why Insurance Eligibility Verification Matters?
Verifying a patient’s insurance eligibility before their appointment is essential for both operational efficiency and patient satisfaction.
It helps dental practices avoid billing issues and ensures transparency in treatment costs.
Key Reasons:
- Confirms active coverage before treatment
- Minimizes claim rejections and delays
- Helps provide clear cost estimates to patients
- Saves time for your front desk team

LIIMRASOFT Insurance Eligibility Verification Process
Here’s how LIIMRASOFT streamline and strengthen your dental Insurance eligibility workflow:
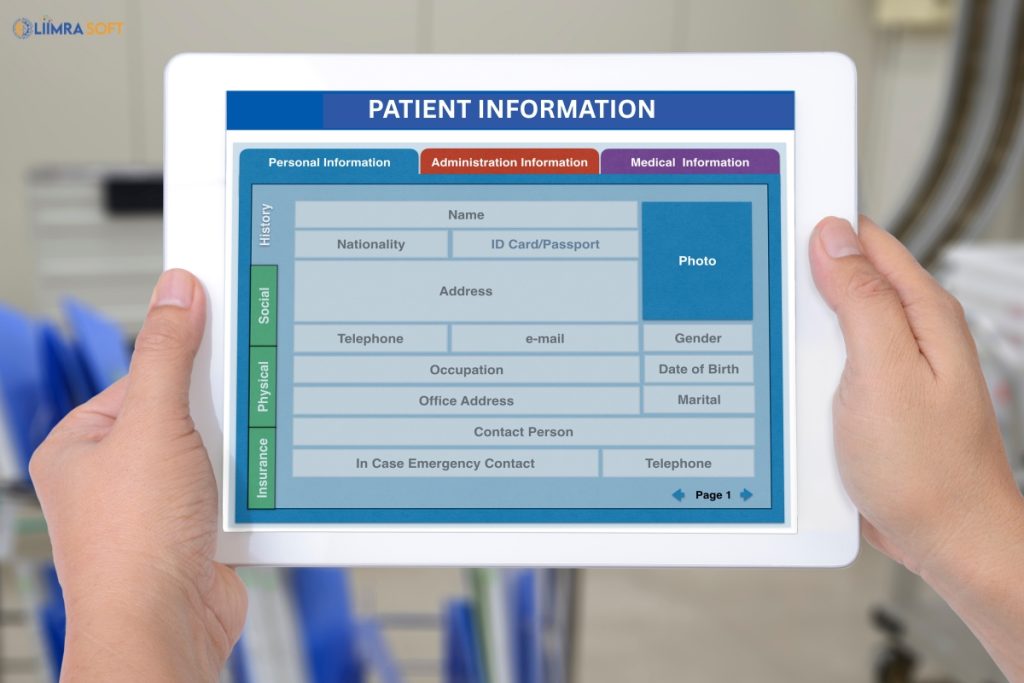
Patient Information Collection
Collecting accurate patient information is the first step in ensuring smooth insurance verification and a hassle-free billing process.
- We collect essential patient information such as full name, date of birth, insurance provider, policy number, and group ID.
- Information is gathered through secure online forms, phone calls, or directly from your practice management system.
- Our team reviews and verifies all details to ensure there are no errors or missing data.
- All patient information is handled in a HIPAA-compliant and confidential manner.
- By managing the data collection process, we free up your front desk staff to focus more on patient care.

Insurance Carrier Communication
- The LIIMRASOFT team actively communicates with insurance carriers to verify real-time benefits and coverage for your patients.
- We use multiple methods—including secure web portals, phone calls, and clearinghouses—to obtain the most accurate and up-to-date information.
- By confirming eligibility, plan details, co-pays, deductibles, and coverage limits in advance, we help prevent claim rejections and billing delays.
- Our proactive approach ensures your practice runs smoothly, improves cash flow, and enhances the patient experience by setting clear expectations upfront.

Comprehensive Verification Report
At LIIMRASOFT, we provide a detailed verification report for each patient to ensure full transparency and preparedness before treatment.
- Confirms if the insurance is active and valid on the date of service.
- Includes information on covered procedures, frequency limits, and any exclusions.
- Shows available annual maximums, deductibles, and co-payments.
- Flags any waiting periods, non-covered services, or plan restrictions.
- Identifies if any treatments need prior approval or referrals.

System Updates & Alerts
- LIIMRASOFT keeps your practice informed by updating your practice management system and alerting your staff to any issues before the patient arrives.
- Whether it’s inactive insurance, missing information, or coverage limitations, we flag potential problems early to help you avoid disruptions during check-in.
- Our proactive notifications allow your team to take corrective action in advance, ensuring a smoother workflow and a better patient experience.
Benefits of LIIMRASOFT Dental Insurance Eligibility Verification Service
Reduce Claim Denials
Catch coverage issues before the claim is submitted.
Improve Front Desk Efficiency
Free up your staff from long hold times and complex insurance portals.
Enhance Patient Experience
Give patients accurate estimates upfront—no billing surprises later.
Speed Up Payment Cycle
Fewer rejections mean faster reimbursements and cleaner billing
HIPAA-Compliant Processes
All patient data is handled securely, with full compliance to privacy regulations.
Who Can Benefit from LIIMRASOFT Services?
LIIMRASOFT’s dental services are designed to support practices of all sizes and specialties. Whether you’re a solo provider or part of a multi-location group, our solutions can help streamline your workflow and improve your revenue cycle.
- General Dentists
- Pediatric Dentists
- Orthodontics
- Periodontics
- Endodontics
- Oral and Maxillofacial Surgeons
- Group and Multi-Location Practices


Why Choose LIIMRASOFT?
- LIIMRASOFT trained dental billing professionals understand the nuances of insurance plans, codes, and provider policies.
- Most verifications completed within 24 hours or sooner.
- LIIMRASOFT adapt to your systems, software, and scheduling process.
- No hidden fees—just reliable service that delivers results.
Start Verifying with Confidence
Stop losing time and money to coverage confusion. Let us take care of eligibility verification so your team can focus on patient care.
Dental Insurance Eligibility Verification
Streamlined dental insurance verification with transparent billing fees you can trust